RUNNING PAIN - A PERSONAL FRUSTRATION

I love running….not only is it a great way to improve cardiovascular health and muscle tone but for me, it’s my “thinking” time.
So, running is great until you get an injury. Right now, I have an issue with my iliotibial band (ITB) after pushing a longer distance. With the goal of running a half marathon, I’m filled with frustration and starting to get a little cranky!
Iliotibial band syndrome (ITBS) is currently cropping up a lot in clinic. It is mostly associated with runners but can also plague road cyclists and rowers. So, I guess I’m not alone….
I thought I would explain a little about what ITBS is, what the risk factors are and some tips (both personal and from research) to get rid of it for good!
So, what is the ITB?
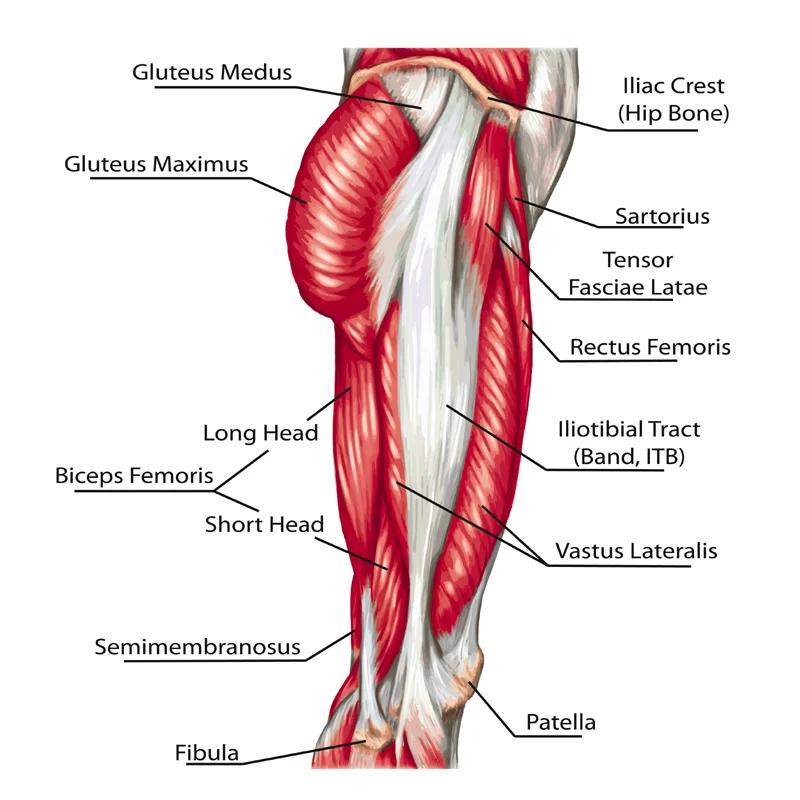
The ITB is a thick band of part fascia, part ligament and part tendon (Geisler and Lazenby, 2017) that runs along the outside of thigh and inserts just below the knee on the tibia (shin bone). It additionally has small attachments to the knee cap, the lateral hamstring and the fibula head (Giangarra and Manske, 2017), (Geisler and Lazenby, 2017). The primary function of the ITB is to help stabilise the hip and knee and to resist the movement of the knee rolling inwards.
Symptoms
Pain is often felt on the outside of the knee and many believe they have a knee injury. Pain is described as intense, burning and / or sharp; exacerbated by running downhill. Now, it was widely understood that friction of the ITB running over the lateral femoral condyl of the femur caused inflammation, but recent research suggests differently. It is now accepted that impingement of a highly innervated fat pad is responsible, so instead of being a friction syndrome it’s now believed to be an impingement zone syndrome. This impingement or compression occurs in the early stance phase, when the knee is bent at approximately 30 degrees. (Grando, et al., 2014).
The biggest risk factor for developing an irritable ITB is increased hip adduction, knee internal rotation and femur external rotation (Noehren, Davis and Hamill, 2007). So, in lay terms outward movement of the thigh, inward movement of the knee and movement of the hip towards the body.
I thought I would share some pointers if you’re experiencing ITB pain:
- I cannot stress enough how important it is to have really good running shoes. Sportlink at Taverham can provide an excellent foot assessment and provide shoes that can support how you run. Remember shoe life is between 350-500 miles and depends on shoe type and gait style.
- Recovery can take up to 6 weeks and I accept this is really frustrating. During the acute phase ice and ibuprofen is important, progressing through the subacute and recovery phase before commencing running again. Mileage should then be kept to below 40 miles a week and speed training is better to start with, adding distance as strength improves (Ramsey, 2016). You may be scratching your head that starting with a faster pace is the correct thing to do! A faster pace is less likely to aggravate the ITB because the time prior to foot release is when the compression occurs. (Brindle, et al., 2014).
- Run on trail instead of road and run somewhere flat for 2 weeks (easy in Norfolk!) to prevent excessive load.
- Research suggests increasing step width may help by reducing strain as this decreases the angle at which the hip inwardly rotates (Brindle, et al., 2014).
- ITBS has often been treated with deep tissue massage, along with stretching exercises. However, research by Faircough, et al., (2006) proposes this is ineffective at reducing symptoms and could potentially exacerbate the problem. This is because the ITB is a really tough structure and no amounts of thumb poking (!!) will change its design.
- Rolling the ITB also has mixed reviews. I did try it initially; it didn’t relieve the symptoms and all I ended up with was rather a lot of bruising. After reading the evidence, I would avoid directly rolling the ITB itself, for the reasons mentioned above. However, rolling the lateral hamstring, TFL and glute maximus would be a better option, purely due to the close bond between these muscles.
- Exercises include strengthening the abductor muscles; so glute medius and glute maximus. An example of a beginner exercise would be a resisted clam, progressing to resisted squat and single leg dead lift (Baker, Souza and Fredericson, 2011).
- Just out of interest, I tried ultrasound and acupuncture (the western kind) with no great results.
Treatment
You could probably say I’m biased, but Osteopathic treatment can really help banish this for good. You could be wondering why, as I’ve said that releasing and stretching the ITB is not effective. Plus ultrasound and acupuncture personally didn’t help. But, it can help as ITBS is a multifactorial issue and not just a problem in the local tissue. (Geisler and Lazenby, 2017). The chain both up and down from this area needs to be assessed and addressed as these tissues and biomechanical flaws can contribute to load transmission. (Geisler and Lazenby, 2017). No one person is the same, so treatment and an exercise programme is completely bespoke to your needs. Sports taping is additionally available to provide some support and enable proprioceptive feedback.
I hope this has helped in terms of understanding why this issue is occurring and ways to manage it. I now need to take some of my own advice and visit an Osteopath!
If you would like any more info, please do not hesitate to contact me at gemma@burevalleyosteopaths.com
Thanks for reading!
Gemma
References
Baker, R., Souza, R. and Fredericson, M. (2011). Iliotibial Band Syndrome: Soft Tissue and Biomechanical Factors in Evaluation and Treatment. PM&R, [online] 3(6), pp.550-561. Available at: https://www.ncbi.nlm.nih.gov/p... [Accessed 10 Jun. 2017].
Brindle, R., Milner, C., Zhang, S. and Fitzhugh, E. (2014). Changing step width alters lower extremity biomechanics during running. Gait & Posture, [online] 39(1), pp.124-128. Available at: https://www.researchgate.net/p... [Accessed 10 Jun. 2017].
Faircough, J., Hayashi, K., Toumi, H., Lyons, K., Bydder, G., Phillips, N., Best, T. and Benjamin, M. (2006). The functional anatomy of the iliotibial band during flexion and extension of the knee: implications for understanding iliotibial band syndrome. Journal of Anatomy, [online] 208(3), pp.309-316. Available at: https://www.ncbi.nlm.nih.gov/p... [Accessed 10 Jun. 2017].
Geisler, P. and Lazenby, T. (2017). Iliotibial Band Impingement Syndrome: An Evidence-Informed Clinical Paradigm Change. International Journal of Athletic Therapy and Training, [online] 22(3), pp.1-11. Available at: https://www.researchgate.net/p... [Accessed 10 Jun. 2017].
Giangarra, C. and Manske, R. (n.d.). Clinical orthopaedic rehabilitation. 4th ed. Philadelphia: Elsevier.
Grando, H., Chang, E., Chen, K. and Chung, C. (2014). MR Imaging of Extrasynovial Inflammation and Impingement About the Knee. Magnetic Resonance Imaging Clinics of North America, [online] 22(4), pp.725-741. Available at: https://www.ncbi.nlm.nih.gov/p... [Accessed 10 Jun. 2017].
Noehren, B., Davis, I. and Hamill, J. (2007). ASB Clinical Biomechanics Award Winner 2006. Clinical Biomechanics, [online] 22(9), pp.951-956. Available at: https://www.researchgate.net/p... [Accessed 10 Jun. 2017].
Ramsey, C. (2016). Running from Iliotibial Band Syndrome: A Guide for Preventing Overuse Injuries. Strategies, [online] 29(2), pp.27-33. Available at: https://www.researchgate.net/p... [Accessed 10 Jun. 2017].
Tagged in:
